Food addiction affects millions of Americans, creating cycles of compulsive eating that feel impossible to break. The condition goes beyond simple willpower issues and requires targeted strategies for lasting change.
We at Amity Palm Beach understand that food addiction and recovery involve complex psychological and physical factors. This guide provides evidence-based approaches to help you regain control over your relationship with food.
What Does Food Addiction Actually Look Like
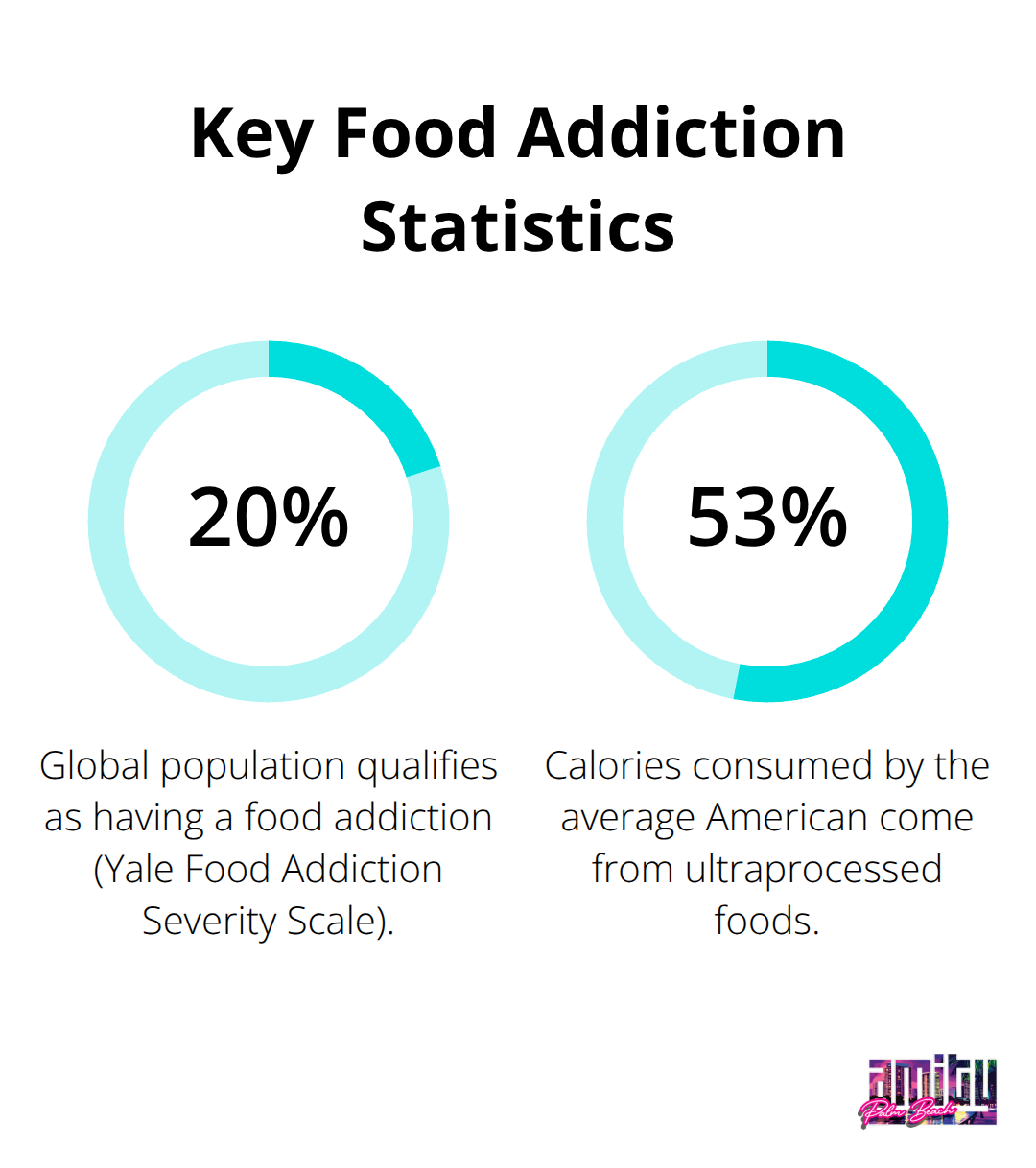
Food addiction manifests through specific behavioral patterns that go far beyond occasional overeating. Research using the Yale Food Addiction Severity Scale shows approximately 20% of the global population qualifies as having a food addiction. The most telling sign involves eating despite physical discomfort or when not hungry, accompanied by intense guilt afterward. People with food addiction experience powerful cravings for specific foods, particularly ultra-processed items high in sugar, fat, and salt. They continue to eat these trigger foods despite negative consequences like weight gain, health problems, or social embarrassment.
Physical Signs That Demand Attention
The physical impact of food addiction extends beyond weight changes. Studies indicate that 53 percent of calories consumed by the average American come from ultraprocessed foods. This excessive consumption leads to disrupted hunger signals, which makes it difficult to recognize true satiety. Common physical symptoms include eating to the point of stomach pain, experiencing withdrawal-like symptoms when avoiding certain foods, and needing increasingly larger portions to achieve satisfaction.
Medical complications often include type 2 diabetes, joint problems, and cardiovascular issues that develop more rapidly than in typical overeating cases.
Mental Health Connections Run Deep
Food addiction rarely exists in isolation from other mental health conditions. Depression and anxiety disorders frequently co-occur with compulsive eating behaviors, which creates a cycle where emotional distress triggers food binges. These binges then increase shame and worsen mental health symptoms. The brain responds to highly processed foods similarly to addictive substances like cocaine, affecting dopamine pathways and creating genuine chemical dependency. This neurological similarity explains why willpower alone fails for most people who struggle with food addiction.
Behavioral Patterns That Signal Trouble
Secret eating behaviors often accompany food addiction, where individuals hide their consumption from family and friends. Many people report feeling powerless over their eating behaviors despite exhibiting strong willpower in other life areas. Binge episodes typically involve consuming unusually large amounts of food within short time periods, followed by feelings of shame and isolation. These patterns create a destructive cycle that becomes increasingly difficult to break without proper intervention and support systems.
How Do You Build Real Recovery Habits
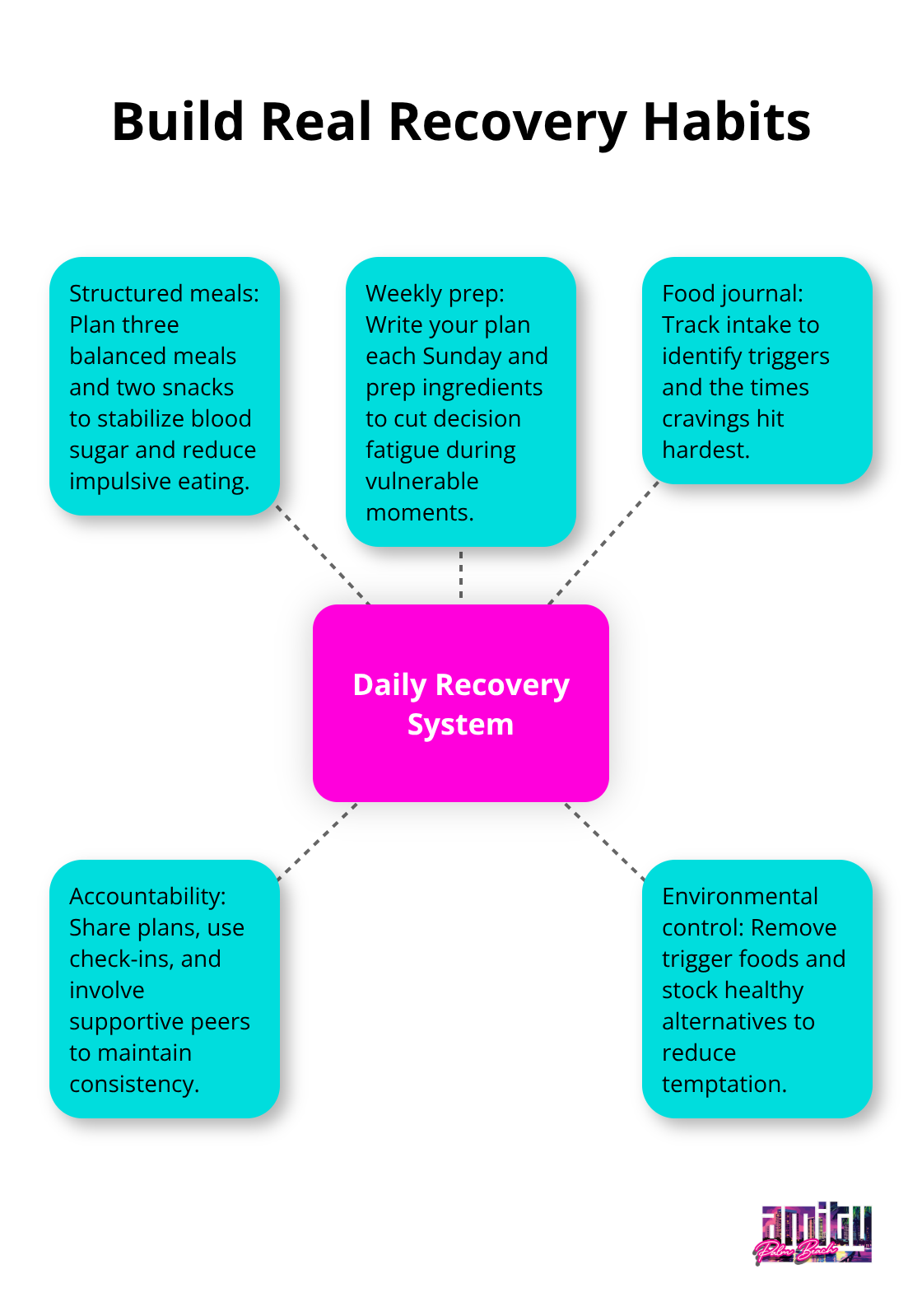
Food addiction recovery demands systematic changes to your daily routines and strong support networks. The most effective approach combines structured meal plans with accountability systems that stop impulsive food choices. Research shows that people who plan their meals eat fewer ultra-processed foods and face fewer cravings throughout the day.
Plan three balanced meals and two snacks daily, with whole foods that keep blood sugar stable. Write your meal plan each Sunday and prep ingredients ahead of time to avoid decision fatigue when you feel vulnerable. Track what you eat in a food journal to spot specific triggers and times when cravings hit hardest.
Create Support Networks That Actually Work
Support systems beat willpower alone for long-term recovery success. Organizations like Food Addicts in Recovery Anonymous and Overeaters Anonymous offer structured programs similar to Alcoholics Anonymous, with both in-person and online meetings at no cost. Find an accountability partner who gets food addiction and schedule daily check-ins during your first 90 days of recovery.
Share your meal plans with trusted family members or friends who can encourage you without judgment. Professional support from therapists who specialize in food disorders adds clinical expertise to your peer support network (this combination proves more effective than either approach alone).
Stop Emotional Triggers Before They Start
Emotional episodes need immediate intervention strategies rather than reactive responses. Identify your top three emotional triggers through daily notes, then develop specific responses for each situation. Replace food-based comfort with alternative activities like phone calls to friends, walks, or deep breathing exercises.
Write a list of pros and cons about quitting trigger foods and carry copies with you as constant motivation. When cravings hit, wait 20 minutes before you act, as most intense urges fade within this timeframe (studies show this delay technique works for 70% of people with food addiction).
Remove Temptation From Your Environment
Stock your space with healthy alternatives and remove trigger foods completely from your home to reduce temptation during weak moments. This environmental control strategy works better than relying on self-control when you face stress or difficult emotions.
Professional treatment programs offer additional tools and medical support that complement these self-help strategies, providing comprehensive approaches to food addiction recovery. Aftercare programs help maintain consistent participation and build lasting recovery habits through ongoing support.
What Professional Treatment Actually Delivers
Professional treatment transforms food addiction recovery through proven therapeutic approaches that address both brain chemistry and behavioral patterns. Enhanced Cognitive Behavioral Therapy stands as the gold standard, with clinical studies that show 60-80% success rates for binge-eating disorder when combined with medical support. This approach rewires thought patterns that trigger compulsive eating while it builds practical coping strategies for high-risk situations. Dialectical Behavioral Therapy adds emotion regulation skills that stop stress-driven food binges before they start. Family-based treatment involves loved ones in meal supervision and accountability, which doubles recovery success rates compared to individual therapy alone.
Medical Support Changes Everything
Medical professionals monitor electrolyte imbalances, heart problems, and bone density issues that food addiction creates over time. Registered dietitians design personalized meal plans that correct nutritional deficiencies while they prevent the restrictive dieting that triggers binge cycles. Antidepressants like selective serotonin reuptake inhibitors show evidence for treating eating disorders when combined with therapy. Regular health monitoring catches complications early and adjusts treatment protocols based on your specific medical needs rather than generic approaches.
Residential Programs Break the Cycle Completely
Residential treatment removes you from trigger environments while it provides 24/7 medical supervision and structured meal times. Day treatment programs offer intensive therapy during business hours while they allow you to return home each evening, which works for people with work or family obligations. These programs combine individual counseling, group therapy sessions, and nutritional education in coordinated treatment plans that address food addiction as a complex medical condition rather than a willpower problem.
Specialized Therapy Approaches That Work
Cognitive Behavioral Therapy targets the specific thought patterns that lead to compulsive eating episodes. Therapists help you identify automatic thoughts like “I’ve already ruined my diet today” that justify continued binge eating. The therapy teaches you to challenge these thoughts and develop healthier responses to food cravings.
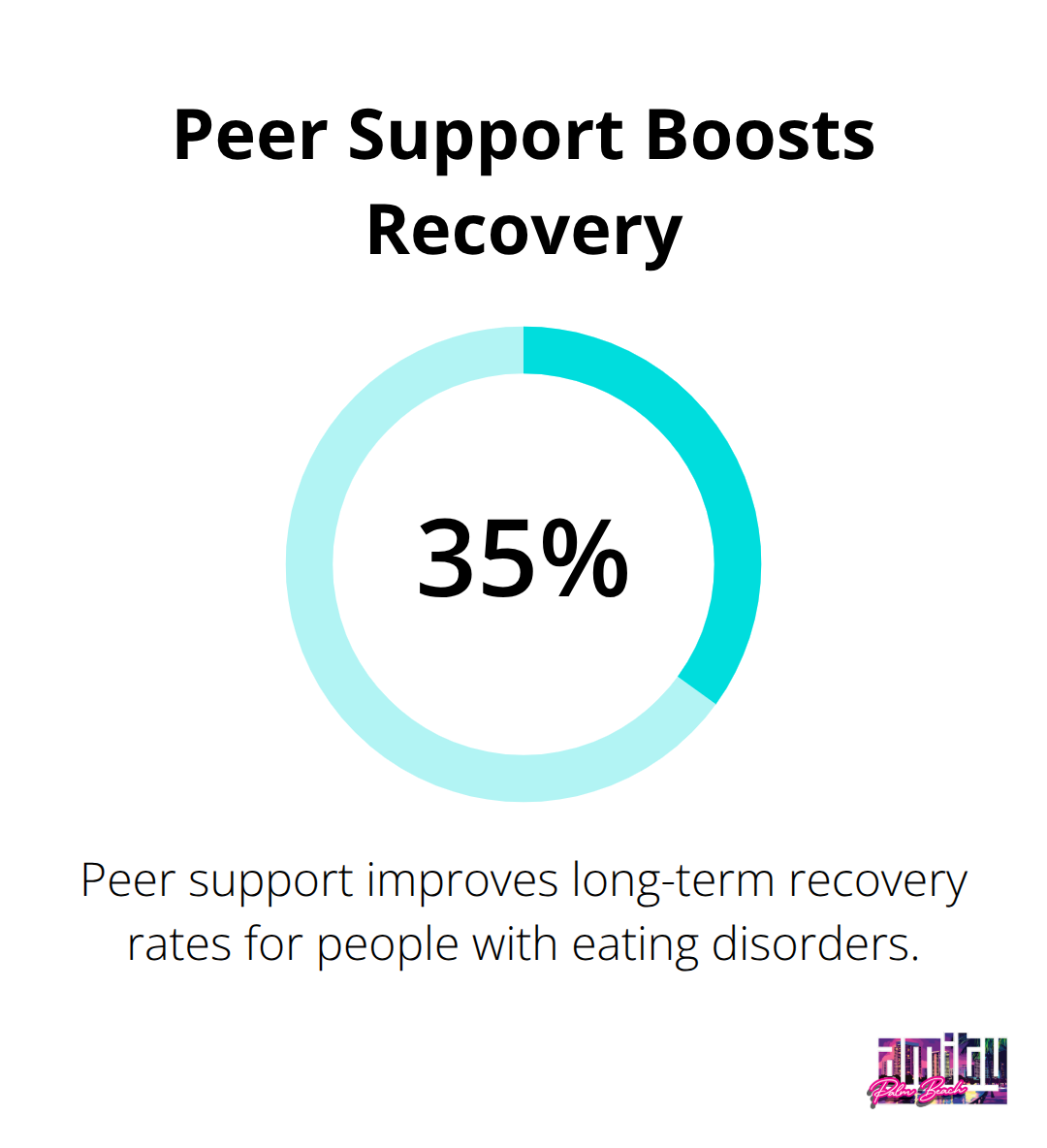
Group therapy sessions connect you with others who face similar struggles, which reduces the isolation that often accompanies food addiction (studies show peer support improves long-term recovery rates by 35%).
Final Thoughts
Food addiction and recovery require commitment, professional support, and evidence-based treatment approaches that address both psychological and physical aspects of the condition. The journey starts with recognition that willpower alone cannot overcome the neurological changes that ultra-processed foods create in your brain. Success depends on structured meal plans, strong support networks, and professional intervention that work together.
Enhanced Cognitive Behavioral Therapy shows 60-80% success rates when paired with medical supervision and nutritional counseling. Organizations like Food Addicts in Recovery Anonymous provide peer support that improves long-term outcomes by 35%. Recovery becomes sustainable through environmental changes, trigger management, and accountability systems (medical supervision prevents dangerous complications while registered dietitians correct nutritional deficiencies that fuel cravings).
We at Amity Palm Beach understand that food addiction often co-occurs with depression, anxiety, and trauma. Our comprehensive treatment approach combines evidence-based therapies with holistic care in supportive environments. The first step involves professional assessment, and recovery is possible when you have the right clinical support and personalized treatment plans.




