Choosing the right addiction treatment requires understanding different care levels and their specific benefits. An accurate inpatient drug rehab definition helps families make informed decisions about recovery options.
We at Amity Palm Beach see many people confused about what inpatient treatment actually involves. This comprehensive guide breaks down the key components, ideal candidates, and essential differences from other treatment approaches.
What Does Inpatient Drug Rehab Actually Include
Inpatient drug rehab treatment means patients live full-time at a residential facility while they receive intensive addiction care. Patients stay at the treatment center 24 hours a day, typically for 30 to 90 days, with medical staff who provide round-the-clock supervision and support. This residential approach removes individuals from their usual environment and triggers while it offers immediate access to medical intervention when withdrawal or mental health crises occur. Treatment centers focus on providing comprehensive residential care, with medical detoxification as the standard first step for most patients who enter inpatient programs.
Medical Care and Safety Protocols
The medical component sets inpatient treatment apart from other recovery options. Board-certified physicians and registered nurses monitor patients continuously as they manage withdrawal symptoms and medication protocols. This level of medical supervision becomes vital when facilities treat substances like alcohol, benzodiazepines, or opioids, where withdrawal can cause life-threatening complications. Facilities typically conduct comprehensive medical evaluations within the first 24 hours, and they assess physical health, substance use history, and co-occurring mental health conditions. The medical team adjusts treatment plans daily based on patient progress and health needs that emerge.
Structured Programming and Daily Routines
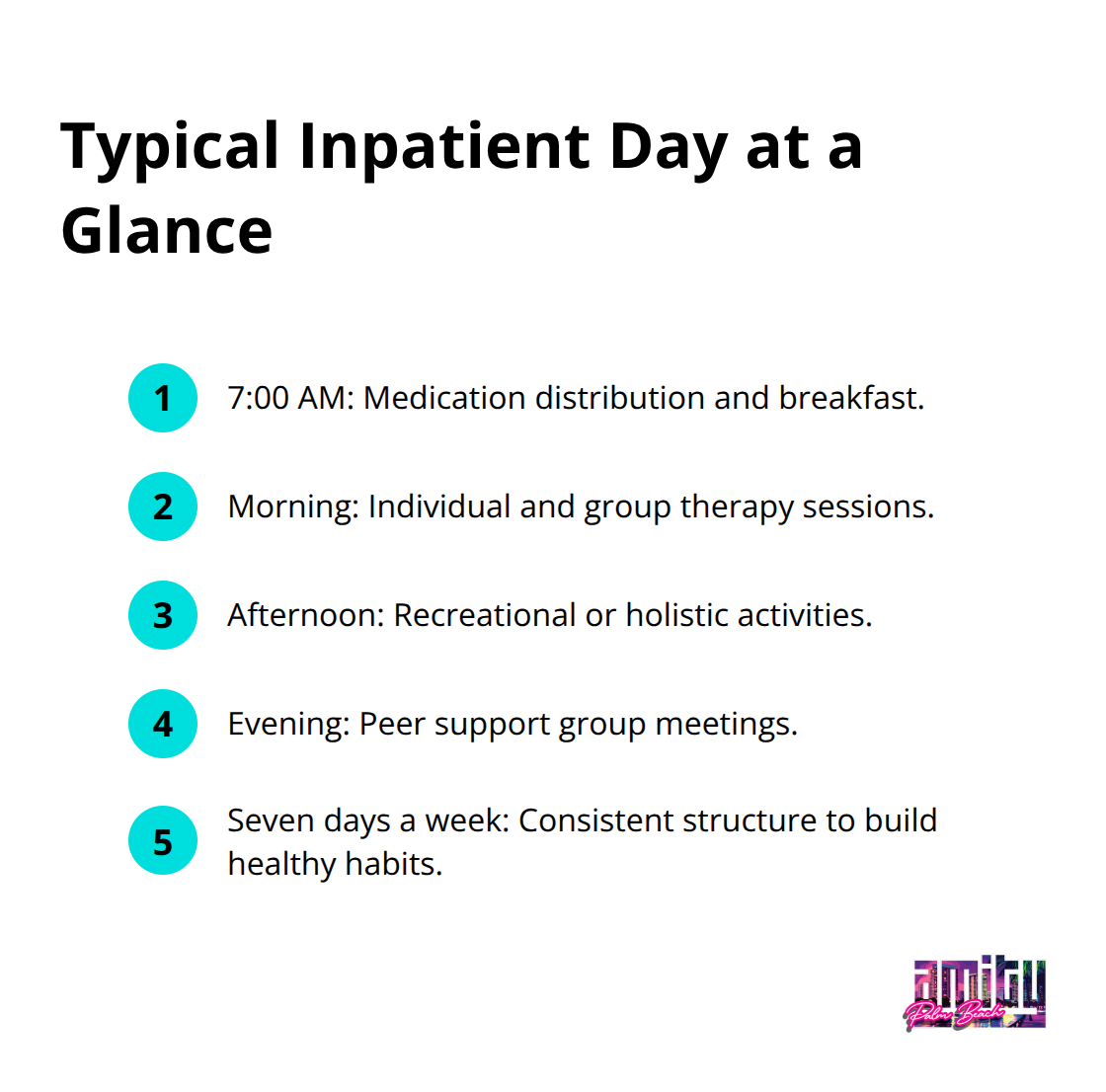
Inpatient programs follow rigid daily schedules that eliminate the chaos often present in active addiction. Patients participate in multiple therapy sessions daily, which include individual counseling, group therapy, and educational workshops about addiction and recovery skills. Most programs begin each day around 7 AM with medication distribution and breakfast, followed by morning therapy sessions, afternoon recreational or holistic activities, and evening support group meetings. This structure continues seven days a week and creates predictable routines that help rewire addictive behavioral patterns while patients build healthy habits.
Key Differences from Outpatient Care
The fundamental difference lies in intensity and environment control. While outpatient treatment allows patients to return home each day, inpatient care provides complete separation from external stressors and substance access. Outpatient programs typically involve 3-9 hours of treatment per week, whereas inpatient care delivers 40-60 hours weekly of therapeutic intervention. More intensive levels like inpatient treatment tend to have higher completion rates than less intensive outpatient programs. Patients with multiple failed outpatient attempts or co-occurring mental health disorders show significantly better outcomes in residential settings where medical and psychological support remains constantly available.
These comprehensive services work together to address the complex nature of addiction, but success depends heavily on specific treatment components that form the foundation of effective inpatient care.
Core Components of Inpatient Drug Rehab
Medical Detox Sets the Foundation
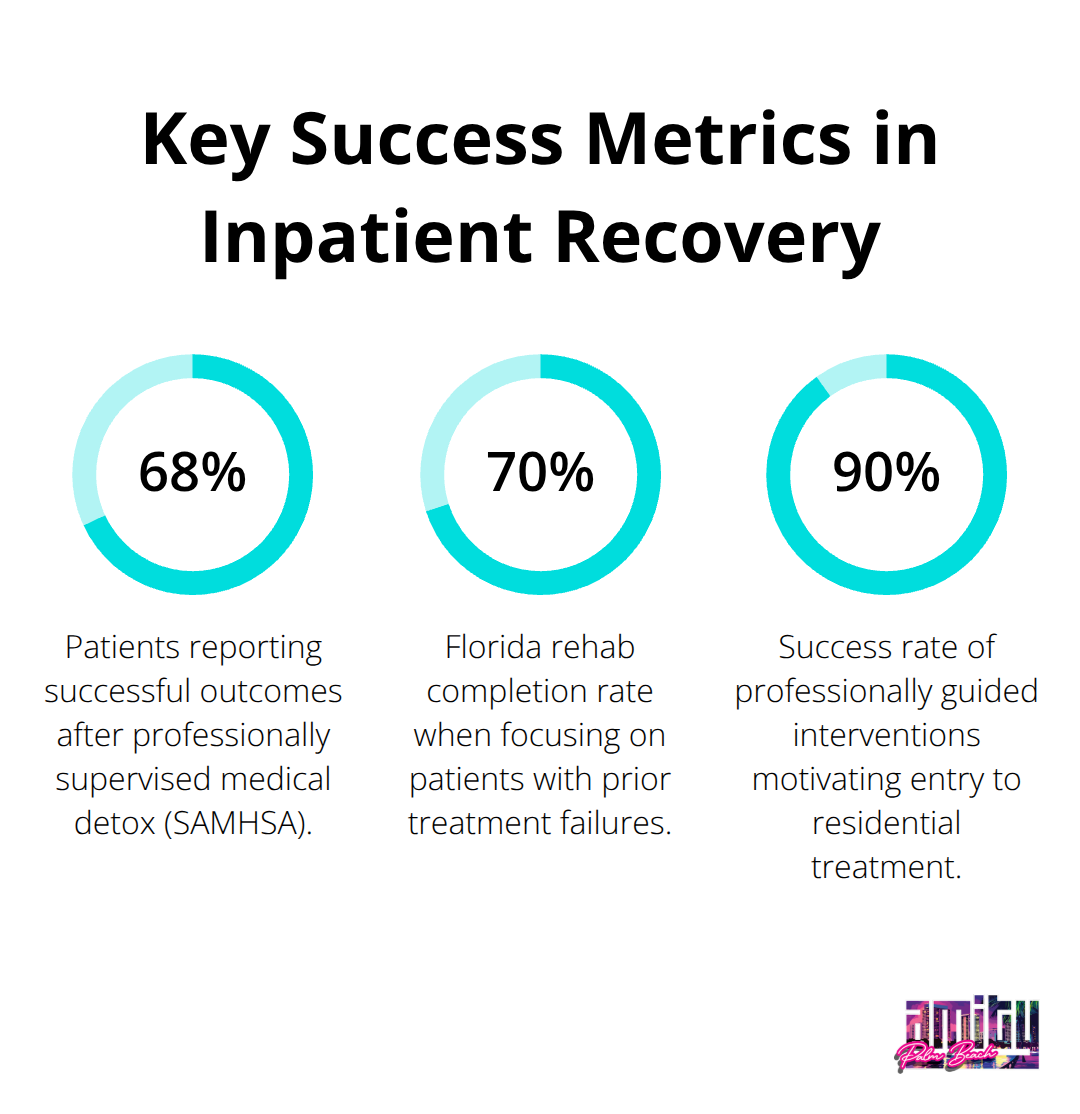
Medical detoxification forms the cornerstone of effective inpatient treatment, with 68% of patients reporting successful outcomes after completing professionally supervised detox programs (according to SAMHSA data). The process involves 24-hour medical monitoring by board-certified physicians and registered nurses who administer FDA-approved medications to manage withdrawal symptoms safely. Facilities use standardized protocols like the Clinical Institute Withdrawal Assessment to track symptom severity and adjust medication dosages every few hours. Most detox programs last 5-10 days, though benzodiazepine withdrawal can require 2-3 weeks of careful tapering to prevent seizures or cardiac complications.
Individual and Group Therapy Drive Recovery
Individual and group therapy sessions consume 6-8 hours daily in quality inpatient programs, with cognitive behavioral therapy and dialectical behavior therapy showing the strongest evidence for addiction recovery. Licensed clinicians conduct one-on-one sessions 3-5 times weekly to address underlying trauma, develop coping strategies, and create personalized relapse prevention plans. Group therapy occurs twice daily and teaches patients communication skills while they practice accountability in a structured peer environment. Facilities that integrate trauma-informed care see higher completion rates than traditional programs, as most patients who enter treatment have experienced significant psychological trauma that fuels their substance use patterns.
Holistic Methods Accelerate Recovery
Modern inpatient facilities incorporate experiential therapies like art therapy, equine-assisted treatment, and adventure therapy to engage different parts of the brain affected by addiction. These approaches activate neuroplasticity mechanisms that traditional talk therapy alone cannot reach, and they help patients rebuild healthy reward pathways damaged by chronic substance use. Yoga and meditation programs reduce cortisol levels by up to 30% within two weeks of consistent practice, while nutritional therapy addresses the vitamin deficiencies and metabolic dysfunction common in active addiction. Exercise therapy programs increase endorphin production naturally and provide patients with sustainable mood regulation tools they can use long after they leave treatment.
These comprehensive treatment components work together to create an intensive therapeutic environment, but the question remains: which patients benefit most from this level of intensive care versus other treatment options?
Who Needs Inpatient Drug Rehab Most
High-Risk Medical Conditions Require 24-Hour Care
Patients who withdraw from alcohol, benzodiazepines, or synthetic opioids face potentially fatal complications that outpatient programs cannot safely manage. Alcohol withdrawal triggers seizures or delirium tremens with mortality rates that reach 15% without proper medical intervention, while benzodiazepine withdrawal causes cardiac arrhythmias and respiratory depression. Individuals who use multiple substances simultaneously need intensive care as drug interactions create unpredictable withdrawal patterns.
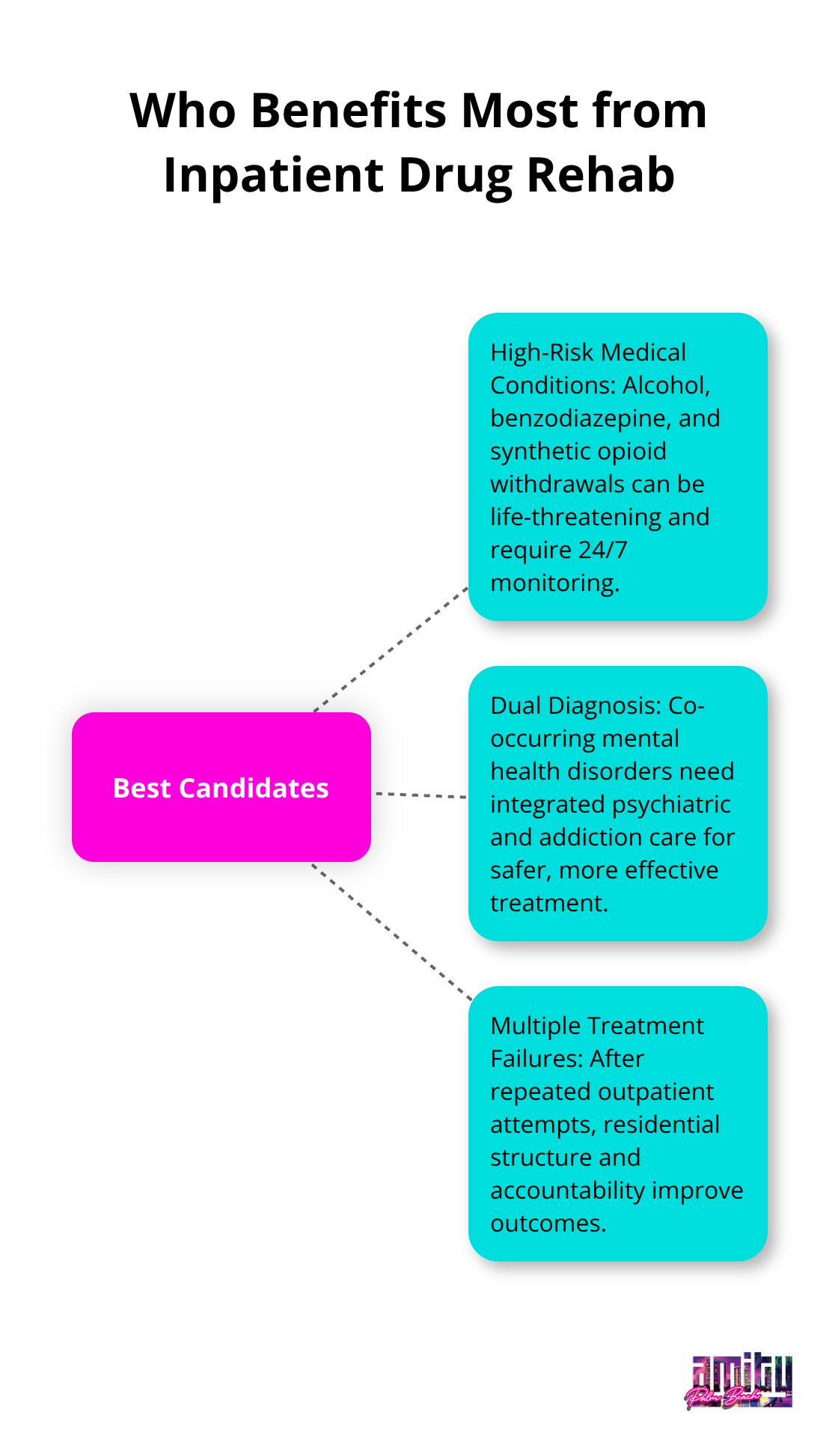
The National Institute on Drug Abuse reports that people with severe opioid use disorder show 35-45% success rates in residential treatment compared to just 15-20% in outpatient settings. Medical professionals intervene immediately when complications arise and prevent life-threatening emergencies that would require hospital transfer from outpatient facilities.
Dual Diagnosis Patients Need Integrated Treatment Teams
Co-occurring mental health disorders affect 48% of inpatient detox patients, and these individuals require specialized care that most outpatient programs cannot provide. Depression, anxiety, PTSD, and bipolar disorder often fuel substance use as self-medication, which makes simultaneous treatment essential for recovery success.
Patients with dual diagnoses show completion rates of only 8.5% in standard programs, but residential facilities with integrated psychiatric care achieve rates above 60%. Board-certified psychiatrists adjust psychiatric medications safely while patients undergo addiction treatment and prevent dangerous drug interactions or mental health crises. The controlled environment allows clinicians to observe how mental health symptoms change as substances leave the system and leads to more accurate diagnoses and effective treatment plans.
Multiple Treatment Failures Indicate Need for Higher Intensity
Individuals who have completed two or more outpatient programs without sustained sobriety need the structure and accountability that only residential treatment provides. Failed outpatient attempts often indicate environmental triggers, social pressures, or co-occurring disorders that require removal from daily stressors.
Florida maintains the highest rehab completion rate at 70% specifically because facilities focus on patients with previous treatment failures who need intensive intervention. The Washington University School of Medicine found that professionally guided interventions have 90% success rates in motivation for people to enter residential treatment after outpatient failures. Patients who remain in residential treatment for at least 90 days show dramatically reduced relapse rates post-discharge compared to those who leave earlier or attempt outpatient care again.
Final Thoughts
A clear inpatient drug rehab definition empowers families to select the right care level for sustained recovery. Inpatient treatment delivers 24-hour medical supervision, structured therapeutic programs, and complete environmental control that outpatient options cannot provide. Medical detox, intensive therapy, and holistic approaches address addiction’s complex nature through comprehensive residential care.
Patients with severe substance use disorders, co-occurring mental health conditions, or multiple treatment failures achieve better outcomes in residential settings. Professional assessment determines the appropriate treatment intensity based on medical history, substance use patterns, and psychological factors. This evaluation prevents inadequate care that leads to relapse or excessive treatment that wastes valuable resources.
We at Amity Palm Beach provide evidence-based treatment through our residential programs (with board-certified physicians and licensed therapists who deliver the medical supervision that defines quality care). Our team combines proven therapeutic methods with personalized approaches to support each patient’s recovery journey. Contact us today to begin your path toward professional assessment and effective treatment.




