Many people entering outpatient addiction treatment wonder: does outpatient rehab drug test patients? The answer is yes, and testing plays a vital role in supporting recovery success.
We at Amity Palm Beach use drug testing as a tool to help patients stay accountable and track their progress. Testing helps treatment teams adjust care plans and provide additional support when needed.
Why Do Outpatient Programs Test for Drugs
The Medical Foundation for Testing
The American Society of Addiction Medicine considers drug testing medically necessary for effective outpatient treatment. Testing serves three primary purposes: it monitors treatment compliance, detects potential relapse early, and adjusts care plans based on objective data rather than self-reports alone.

The Substance Abuse and Mental Health Services Administration reports that drug testing significantly improves treatment outcomes when programs combine it with clinical evaluations. Programs typically test for the most commonly abused substances including THC, cocaine, opioids, amphetamines, and alcohol metabolites. Many facilities also screen for benzodiazepines (which standard panels often miss despite their high abuse potential).
How Testing Creates Treatment Accountability
Testing frequency varies based on risk assessment. High-risk patients face testing up to four times yearly while low-risk individuals may undergo annual screening. The National Institute on Drug Abuse found that patients aware of random testing show lower relapse rates compared to those in programs without testing protocols.
Urine remains the preferred testing method due to its 30-day detection window and cost-effectiveness at roughly $25-50 per test. Hair follicle testing costs more but can detect substance use up to 90 days prior and prevents most attempts at test manipulation.
Trust Through Transparent Monitoring
Testing rebuilds damaged relationships by providing objective proof of sobriety to family members and employers. The Federation of State Medical Boards emphasizes unannounced testing as the gold standard because it prevents patients from timing substance use around known test dates.
Modern confirmation laboratories use mass spectrometry to deliver high accuracy rates, which eliminates the false positives common with basic cup tests. This precision allows treatment teams to make informed decisions about medication adjustments, therapy intensity, and discharge planning based on concrete evidence rather than assumptions.
The next phase of treatment involves understanding addiction recovery exactly when and how often these tests occur throughout your recovery journey.
How Often Will You Be Tested
Testing Frequency Changes Throughout Treatment
Outpatient programs adjust testing frequency based on your treatment phase and risk level. During the first 30 days of intensive outpatient programs, most facilities conduct tests twice weekly to establish baseline sobriety and medication compliance. Research shows that longer treatment models of 18 months or more demonstrate better results in reducing substance use, which allows teams to intervene before full addiction returns.
Partial hospitalization programs test daily during the first week, then transition to every other day through week four. After 90 days of consistent negative results, testing typically drops to weekly intervals. Patients with co-occurring mental health disorders face more frequent testing because psychiatric medications can interact dangerously with substances (creating medical emergencies that require immediate detection).
Random Testing Beats Scheduled Appointments
Random testing protocols prove far more effective than predictable schedules. Clinical guidelines emphasize that appropriate drug testing helps identify, diagnose, treat, and support recovery for patients. Most programs implement a mixed approach: scheduled tests during medical appointments plus random calls that require testing within 24 hours.
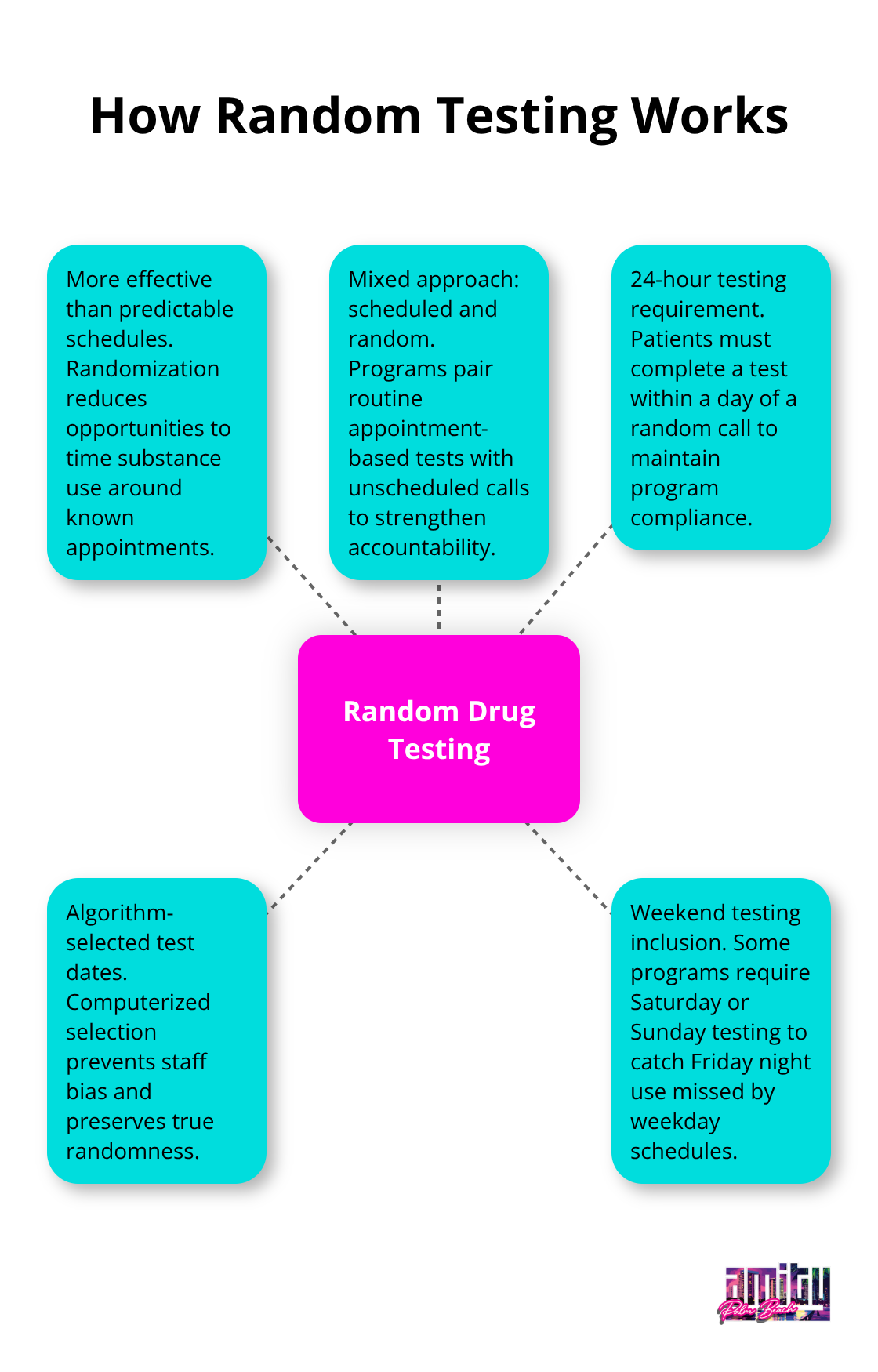
High-risk patients face random testing up to four times monthly, while stable patients undergo monthly random screens. Programs use computer algorithms to select test dates, which prevents staff bias and maintains true randomness. Some facilities require weekend testing to catch Friday night substance use (which standard Monday-Friday schedules miss entirely).
Your Risk Level Determines Testing Schedule
Individual factors heavily influence testing frequency beyond standard protocols. Patients prescribed controlled substances like benzodiazepines or stimulants face twice-weekly testing regardless of treatment phase. Previous treatment failures trigger enhanced monitoring with daily testing for the first two weeks, then gradual reduction based on compliance.
Employment requirements also affect schedules. Healthcare workers and commercial drivers need documentation of sobriety for licensing boards, which requires monthly confirmatory testing with mass spectrometry methods. Patients with legal mandates face court-ordered testing frequencies that override standard medical protocols, often requiring immediate results within hours rather than standard laboratory timeframes.
Understanding these testing schedules helps you prepare for treatment, but what happens when a test comes back positive presents an entirely different set of challenges and opportunities.
What Happens If You Test Positive
Immediate Medical Assessment Takes Priority
A positive drug test triggers immediate medical evaluation at most facilities. Treatment teams assess vital signs, mental status changes, and potential drug interactions with prescribed medications. The American Society of Addiction Medicine emphasizes that positive tests indicate medical instability rather than moral failure, which requires clinical intervention rather than punishment.
Medical staff check for dangerous combinations like alcohol with benzodiazepines or cocaine with heart medications that can cause fatal complications. Patients who take Suboxone and test positive for fentanyl face immediate dose adjustments because these substances create respiratory depression risks when mixed. Blood pressure checks become mandatory for stimulant-positive tests since cocaine and methamphetamines can trigger heart attacks or strokes hours after use.
Treatment Intensification Replaces Discharge Threats
Modern programs respond to positive tests by increasing support rather than removing patients from care. Forced treatment approaches mirror punitive criminalization methods, repackaged as beneficial interventions for people who use drugs. Most accredited programs now require patients to attend additional therapy sessions, increase test frequency to twice weekly, and participate in peer support meetings.
Medication adjustments happen immediately after positive results. Patients on naltrexone may need dose increases, while those who receive Suboxone often require split doses to prevent breakthrough cravings. Treatment teams distinguish between isolated slips and pattern relapses by examining test results over 30-day periods. Single positive tests typically trigger two weeks of daily check-ins, while multiple positives within a month indicate the need for higher levels of care like partial hospitalization programs.
Legal Compliance Versus Medical Treatment
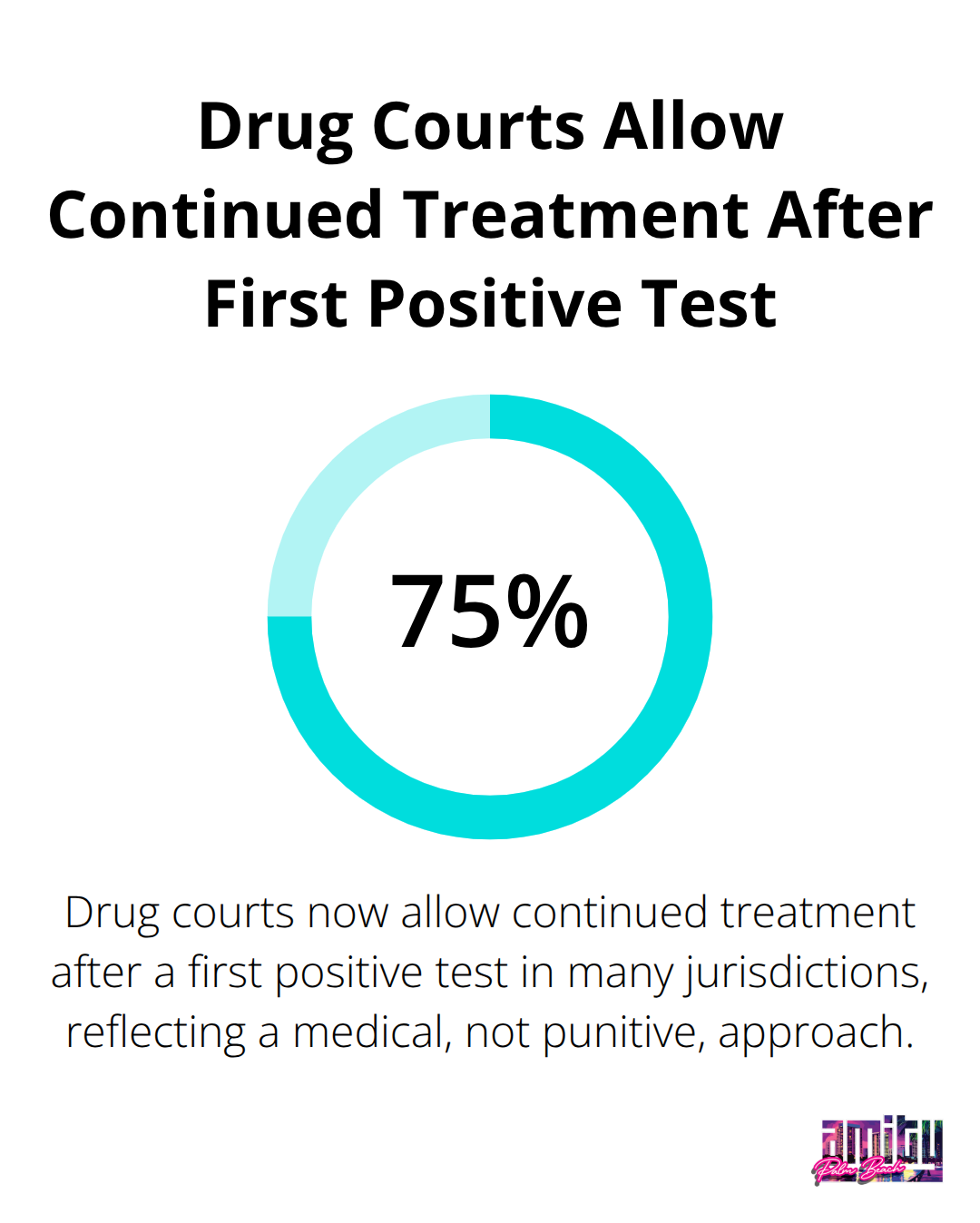
Court-mandated patients face different consequences than voluntary participants. Probation officers receive immediate notification of positive tests, which potentially triggers jail time or extended supervision periods. However, drug courts increasingly recognize that addiction requires medical treatment rather than incarceration, with 75% now allowing continued treatment after first positive tests.
Employment-related tests create separate challenges. Healthcare workers must report positive results to licensing boards within 72 hours (often resulting in temporary practice restrictions). Commercial drivers lose DOT certification immediately after positive tests and require completion of return-to-duty protocols before license restoration. Treatment programs help navigate these professional consequences while they maintain focus on recovery goals rather than career preservation alone.
Final Thoughts
Drug tests form the backbone of successful outpatient recovery programs. The evidence shows clear benefits: patients who undergo regular tests demonstrate higher sobriety rates, improved medication compliance, and stronger long-term outcomes compared to programs without protocols. Tests rebuild trust between patients and their support networks through objective verification rather than promises alone.
The question “does outpatient rehab drug test” reflects legitimate concerns about privacy and autonomy. However, modern programs use tests as supportive tools rather than punishment. Positive results trigger increased medical attention and enhanced therapy rather than program dismissal (which outdated facilities still practice).
We at Amity Palm Beach integrate comprehensive drug tests into our evidence-based treatment approach. Our programs combine medical supervision with personalized care to support your recovery journey. Contact us today for a confidential assessment and learn how our protocols support lasting sobriety.




