Drug rehab relapse rates remain a significant concern for individuals and families navigating addiction recovery. Research shows that 40-60% of people experience relapse after completing treatment programs.
We at Amity Palm Beach understand these statistics can feel overwhelming. However, knowing the factors behind relapse and proven prevention strategies can dramatically improve long-term recovery outcomes.
Current Statistics on Addiction Relapse Rates
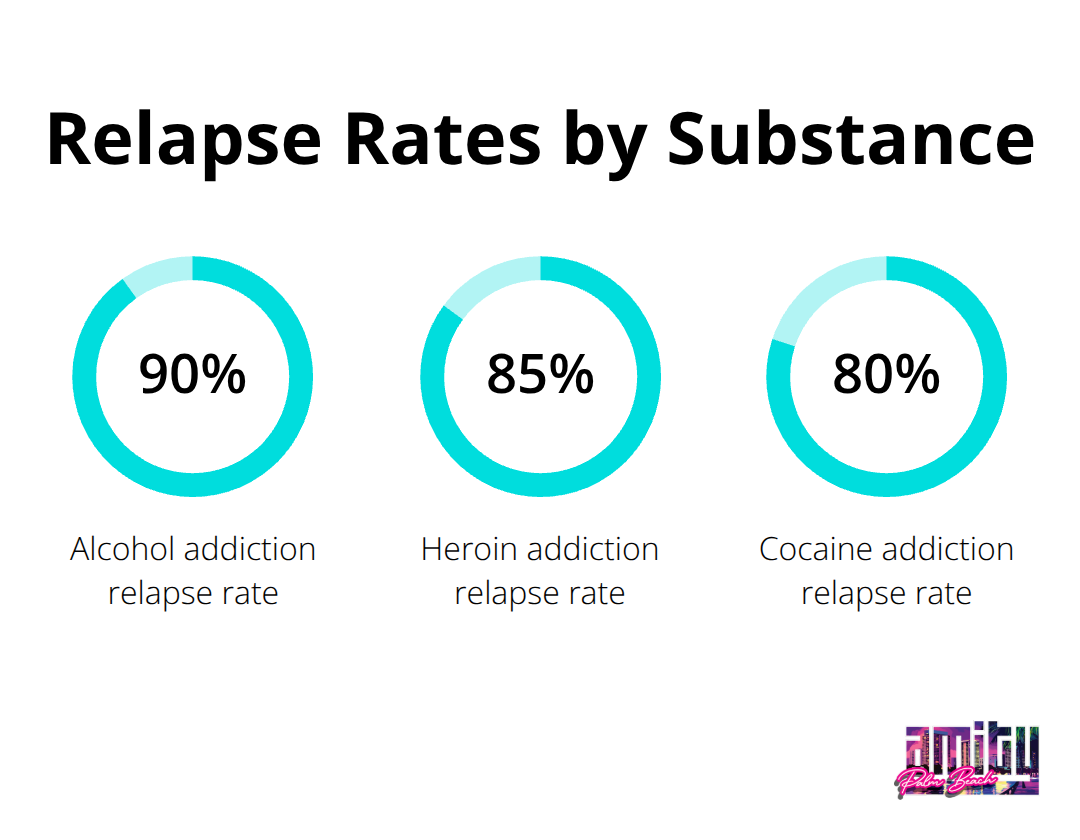
The numbers reveal a stark reality across different substances. Alcohol addiction carries a relapse rate of 90%, while heroin addiction shows an 85% relapse rate according to recent studies. Cocaine addiction demonstrates an 80% relapse rate, which highlights the persistent nature of stimulant dependencies. These figures from the National Institute on Drug Abuse show that addiction recovery involves ongoing challenges regardless of the substance involved.
Timeline Patterns That Matter Most
Most relapses occur within predictable windows. The Substance Abuse and Mental Health Services Administration reports that 40-60% of individuals relapse within 30 days of leaving inpatient treatment. Up to 85% experience relapse within the first year of recovery, with the highest risk period occurring in the first 6-12 months after treatment. However, after 5 years of sustained recovery, relapse rates drop significantly to approximately 15%. This data shows that survival through the first year dramatically improves long-term success odds.
Individual Risk Factors That Create Differences
Personal circumstances create vastly different relapse probabilities. Research from Iran involving 400 male participants found that 85.5% had relapse histories, with peer influence emerging as the strongest behavioral risk factor. Socioeconomic elements like unemployment and low income served as significant predictors of relapse. Early substance use onset proved particularly problematic (nearly 50% of participants began drug consumption before age 20). Mental health conditions, especially untreated depression and anxiety, amplify relapse risk substantially.
Social and Environmental Influences
People with strong family support systems and stable employment show markedly better outcomes than those who face social isolation or financial stress. The social environment significantly influences addiction relapse, where proximity to active users can tempt individuals in recovery. Work-related stress and financial difficulties link to increased risk of relapse, as individuals may revert to substances for escape. These environmental factors interact with personal vulnerabilities to create complex relapse scenarios that treatment programs must address through comprehensive approaches.
Common Causes of Relapse After Treatment
Environmental factors dominate relapse scenarios more than most people realize. Places, people, and situations connected to past substance use create powerful memory triggers that activate cravings within seconds. The brain associates specific locations like bars, former dealer neighborhoods, or even certain friends’ houses with drug use patterns developed over months or years.
Social pressures compound these environmental risks significantly. Research shows that individuals surrounded by active users face relapse rates that exceed 70%, compared to 35% for those in substance-free social circles. Work environments where alcohol culture prevails or where colleagues use substances create constant temptation. Family events where alcohol flows freely can trigger relapses even months after successful treatment completion.
Mental Health Conditions Drive Most Serious Relapses
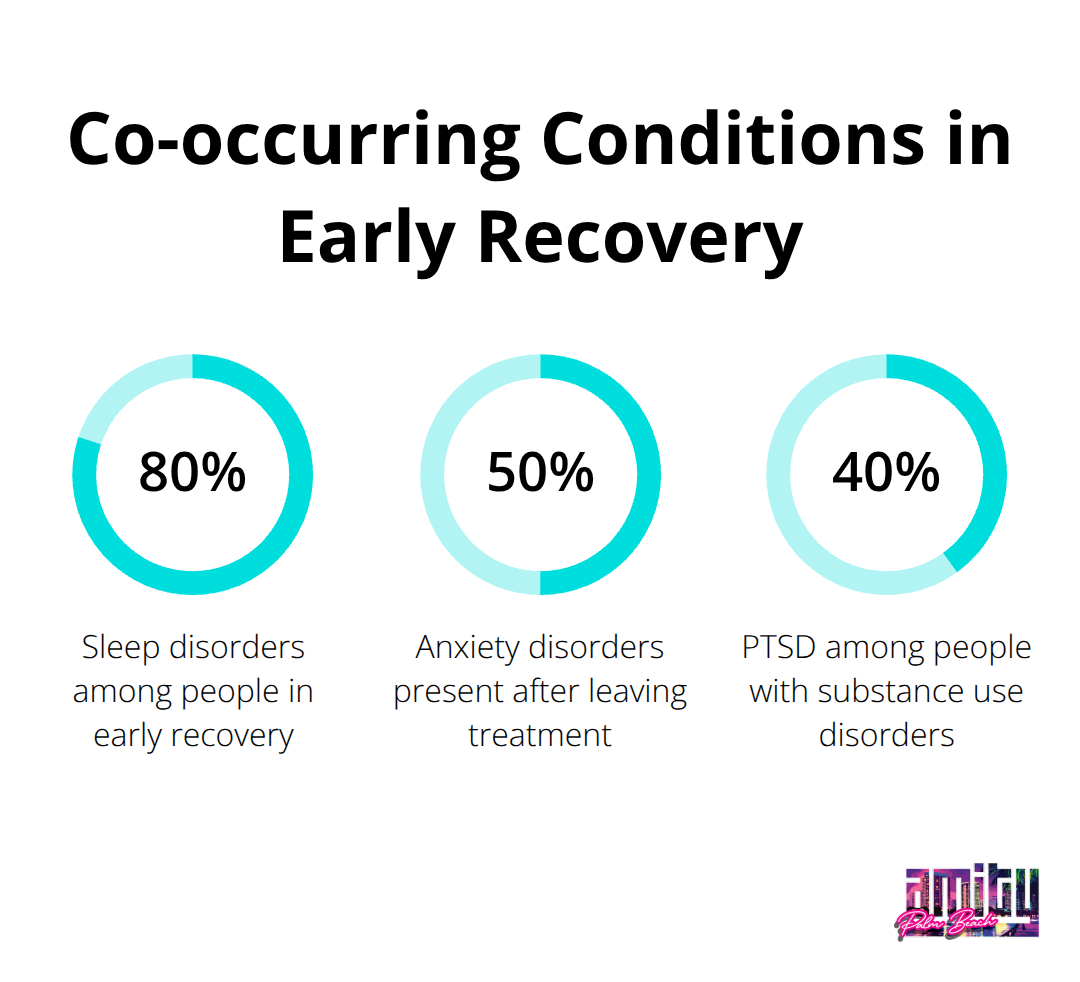
Untreated depression creates complex bidirectional relationships with substance use disorders and serves as a primary relapse predictor according to mental health studies. Anxiety disorders, present in 50% of individuals who leave treatment, create overwhelming urges to self-medicate when left unaddressed. Trauma-related conditions like PTSD affect 40% of people with substance use disorders and generate flashbacks that drive immediate substance-seeking behavior.
Co-occurring bipolar disorder creates manic episodes where judgment becomes severely impaired, which leads to impulsive drug use decisions. Sleep disorders plague 80% of people in early recovery, which creates exhaustion and emotional instability that weakens resistance to substance cravings.
Aftercare Failures Create Predictable Relapse Patterns
Treatment programs often discharge patients without comprehensive aftercare planning, though 85% and 95% of rehab completers report being drug-free nine months later with proper support. Weekly therapy appointments scheduled months in advance leave dangerous gaps when crisis situations arise. Support group recommendations without specific meeting locations and times result in non-attendance rates above 70%.
Medication management failures occur when prescriptions run out and refill appointments get delayed by weeks. Housing instability affects 45% of people who leave residential treatment, which forces them back into substance-using environments where relapse becomes nearly inevitable.
Stress and Emotional Triggers Overwhelm Coping Skills
Work-related stress and financial difficulties link directly to increased relapse risk, as individuals may revert to substances for escape. Relationship conflicts, job loss, or major life changes can overwhelm newly developed coping mechanisms (particularly in the first six months of recovery). Boredom and loneliness prompt substance use when people lack structured activities or meaningful social connections.
Negative emotions like sadness, anger, and frustration can trigger substance cravings when healthy coping strategies remain underdeveloped. The first week after treatment completion proves especially dangerous, as many people relapse to avoid withdrawal symptoms that resurface during stress.
These complex factors interact to create high-risk situations that require comprehensive prevention strategies and ongoing professional support to address effectively.
Strategies to Reduce Relapse Risk
Medication-assisted treatment transforms recovery outcomes when treatment centers integrate it properly with comprehensive care. The National Institute on Drug Abuse reports that FDA-approved medications like naltrexone, buprenorphine, or methadone combined with counseling significantly reduce opioid relapse rates. MAT blocks euphoric effects, reduces cravings, and normalizes brain chemistry that prolonged substance use disrupts. Treatment centers that offer MAT alongside behavioral therapy show dramatically better retention rates than facilities that use abstinence-only approaches. The key lies in viewing medication as a tool rather than a crutch, which requires ongoing medical supervision and gradual tapering protocols.
Building Accountability Networks That Work
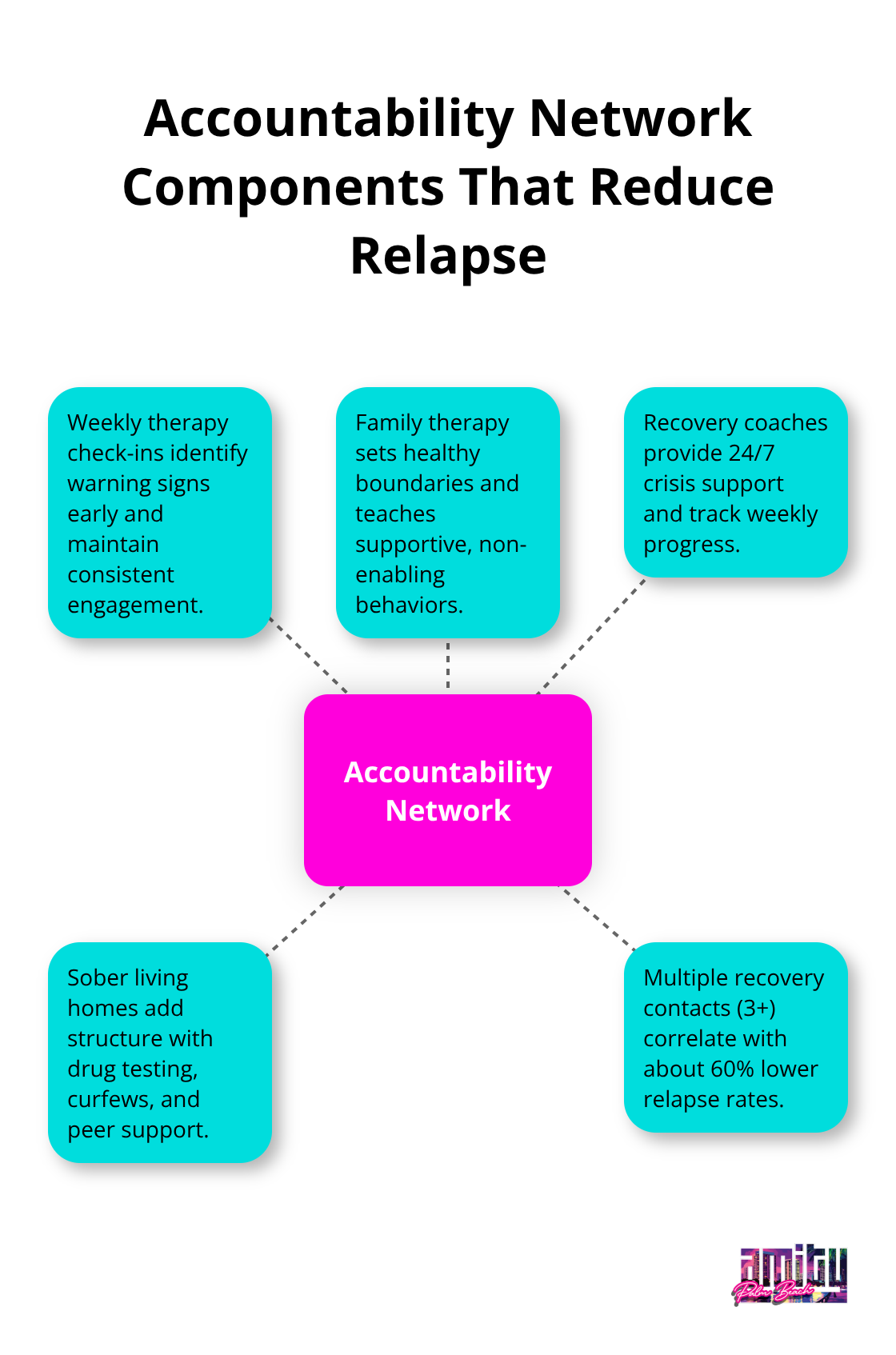
Support systems require specific structure to prevent relapse effectively. Weekly therapy sessions through Alcoholics Anonymous or Narcotics Anonymous create mandatory check-ins that identify warning signs before crisis hits. Family therapy sessions teach relatives how to provide support without enabling destructive behaviors, while they set clear boundaries around consequences. Professional accountability partners like recovery coaches provide 24/7 crisis intervention and weekly progress monitoring. Sober living homes extend this accountability through mandatory drug testing, curfews, and peer support systems that maintain structure beyond residential treatment. Research shows individuals with three or more recovery support contacts have 60% lower relapse rates than those who attempt recovery alone.
Practical Coping Skills That Replace Substance Use
Stress management techniques must become automatic responses before cravings overwhelm decision-making capacity. Mindfulness meditation practiced daily for 20 minutes reduces cortisol levels and strengthens prefrontal cortex function responsible for impulse control. Regular exercise programs that include both cardio and strength training release endorphins that naturally combat depression and anxiety without pharmaceutical intervention. Cognitive Behavioral Therapy teaches specific thought-stopping techniques and behavioral substitutions that interrupt craving cycles within seconds. Sleep hygiene protocols address the 80% of early recovery individuals who experience insomnia (which directly correlates with relapse risk). Financial planning and vocational training provide concrete goals that create meaning beyond substance use, while they establish daily routines that eliminate unstructured time where relapse thoughts typically flourish.
Comprehensive Treatment Approaches That Address Root Causes
Dual diagnosis treatment addresses both addiction and mental health conditions simultaneously rather than treating them as separate issues. Research consistently demonstrates a high rate of co-occurrence between substance use disorders and psychopathology, particularly major depressive disorders. Trauma-informed therapy helps process underlying experiences that drive substance use patterns (particularly important for the 40% of people with substance use disorders who also have PTSD). Holistic therapies like yoga, meditation, and art therapy provide alternative outlets for emotional expression and stress relief. These comprehensive approaches create multiple pathways to recovery success rather than relying on single-method treatment plans.
Final Thoughts
Drug rehab relapse rates present a challenging reality, but these statistics empower better recovery plans. The 40-60% relapse rate within the first year represents evidence that addiction requires ongoing management like other chronic conditions. Success depends on comprehensive treatment that addresses both substance use and underlying mental health conditions.
Medication-assisted treatment, structured aftercare programs, and strong support networks create multiple safety nets that reduce relapse risk significantly. Data shows that individuals who survive the first year of recovery see their relapse rates drop to just 15% after five years. Professional help becomes necessary when warning signs emerge (increased isolation, mood changes, or exposure to high-risk situations).
We at Amity Palm Beach provide evidence-based treatment that combines medical supervision with personalized care. Our integrated approach addresses addiction as a multi-dimensional condition that requires comprehensive treatment to heal body, mind, and spirit. Recovery remains possible for everyone, regardless of previous relapse history.




